What We Lose When We Exclude Continuous Behavioral Measurement in Clinical Research & Practice?
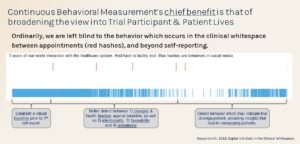
Health condition detection and care are only as good as their measurability against a baseline over time. Mental and behavioral health measurement has traditionally been taken with self-reported surveys and validated scales, like PHQ-9 and GAD-7. Too few mental and behavioral health providers are aware that smartphones, apps, and sensors can continually measure passive behaviors which indicate mental states. This emergent measurement, continuous behavioral health measurement (CBHM), provides richer behavioral insights into the “clinical whitespace” between clinic appointments and beyond self-reporting. Dr. Glenn Coppersmith, in his article, Digital Life Data in The Clinical Whitespace (2022), talks about continuous behavior measurement’s advantages, over self-reporting.
Given this possibility for visibility into the clinical whitespace, we ask why this approach is not universally used as a complement to self-reported surveys and validated scales, like PHQ-9 and GAD-7. When CBHM use is excluded from clinical research and patient care, we lose:
- more effective appointments and stronger therapeutic alliances are lost for lack of richer real-world behavioral insights from the clinical whitespace between appointments and beyond self-reporting,
- broader and richer access to good healthcare is lost because passive behaviors which signal notable declines in health status are missed.
- reduction of more expensive interventions & outcomes, i.e. emergency rooms, hospitalization, suicide, would yield earlier, more timely, and predictable, detection and intervention, and
- more optimal mental and behavioral health intervention combinations due to collection and analysis of richer real-world data across diverse conditions and populations, not just related to mental and behavioral health, but also with acute and chronic conditions where function and quality of life are important outcomes, and
- earlier detection of behavior-related financial, moral, care and regulatory risk factors.
Below is a key image from the Coppersmith (2022) article which highlights the benefit of continuous behavioral measurement, and where you see how much insight is lost when only live appointments are self-reported, note the upper hash marks.
If the losses noted above are part of a list of losses you are looking to avoid in your own clinical research studies or care practice, schedule a demonstration. We would love to discuss how Ksana Health can help improve your outcomes.
Reference:
Coppersmith G. Digital Life Data in the Clinical Whitespace. Current Directions in Psychological Science. 2022;31(1):34-40. doi:10.1177/09637214211068839
1 September 2022
Recent Articles
Enhancing Behavioral Health Care: Insights from the 2023 Society for Digital Mental Health Conference
Contributed by Lauren Weiner, Ksana Health Director of Clinical Science. On June 21, 2023, Ksana Health recently attended the 2023 Society for Digital Mental Health Conference. The event highlighted the role of...
Continue readingKsana Health selected to join the Beyond Language Studio!
Ksana Health is jazzed to be selected to join the Beyond Language Studio, a collaboration between Sorenson and Newlab supporting deep-tech startups building high-impact, innovative products, and services through real-world pilot projects. The...
Continue readingKsana Health 2022 Highlights (in Video)
For Ksana Health, 2022 was a year of perseverance, learning and optimization. We are grateful to all the partners, collaborators and supporters who made the year what it was. The video below...
Continue reading